Deep brain stimulation, utilizing implanted electrodes to deliver electrical pulses, serves as a common treatment for Parkinson’s disease and other neurological disorders. However, these electrodes are prone to corrosion and scar tissue buildup, often necessitating removal. Now, MIT researchers offer a promising alternative: ultrasound. They have developed a method for deep brain stimulation using ultrasound delivered through a fiber no thicker than a human hair. In mice studies, this stimulation successfully triggered dopamine release in a brain area frequently targeted in Parkinson’s patients.
“By using ultrasonography, we can create a new way of stimulating neurons to fire in the deep brain,” explains Canan Dagdeviren, an associate professor in the MIT Media Lab and the senior author of the study. “This device is thinner than a hair fiber, so there will be negligible tissue damage, and it is easy for us to navigate this device in the deep brain.”
This innovative approach not only presents a potentially safer method for deep brain stimulation but also holds immense value for researchers delving into the complexities of the brain.
Published in Nature Communications, the study was led by MIT graduate student Jason Hou and MIT postdoc Md Osman Goni Nayeem, with contributions from collaborators at MIT’s McGovern Institute for Brain Research, Boston University, and Caltech. Dagdeviren’s lab has previously pioneered wearable ultrasound devices capable of delivering drugs through the skin and performing diagnostic imaging on various organs. However, delivering ultrasound deep into the brain from a head-mounted device poses a significant challenge due to the skull’s interference with ultrasound waves.
“If we want to go into the deep brain, then it cannot be just wearable or attachable anymore. It has to be implantable,” Dagdeviren states. “We carefully customize the device so that it will be minimally invasive and avoid major blood vessels in the deep brain.”
While FDA-approved deep brain stimulation with electrical impulses exists for treating Parkinson’s symptoms, the millimeter-thick electrodes used can corrode over time. Additionally, scar tissue accumulation around the implant can hinder electrical impulses.
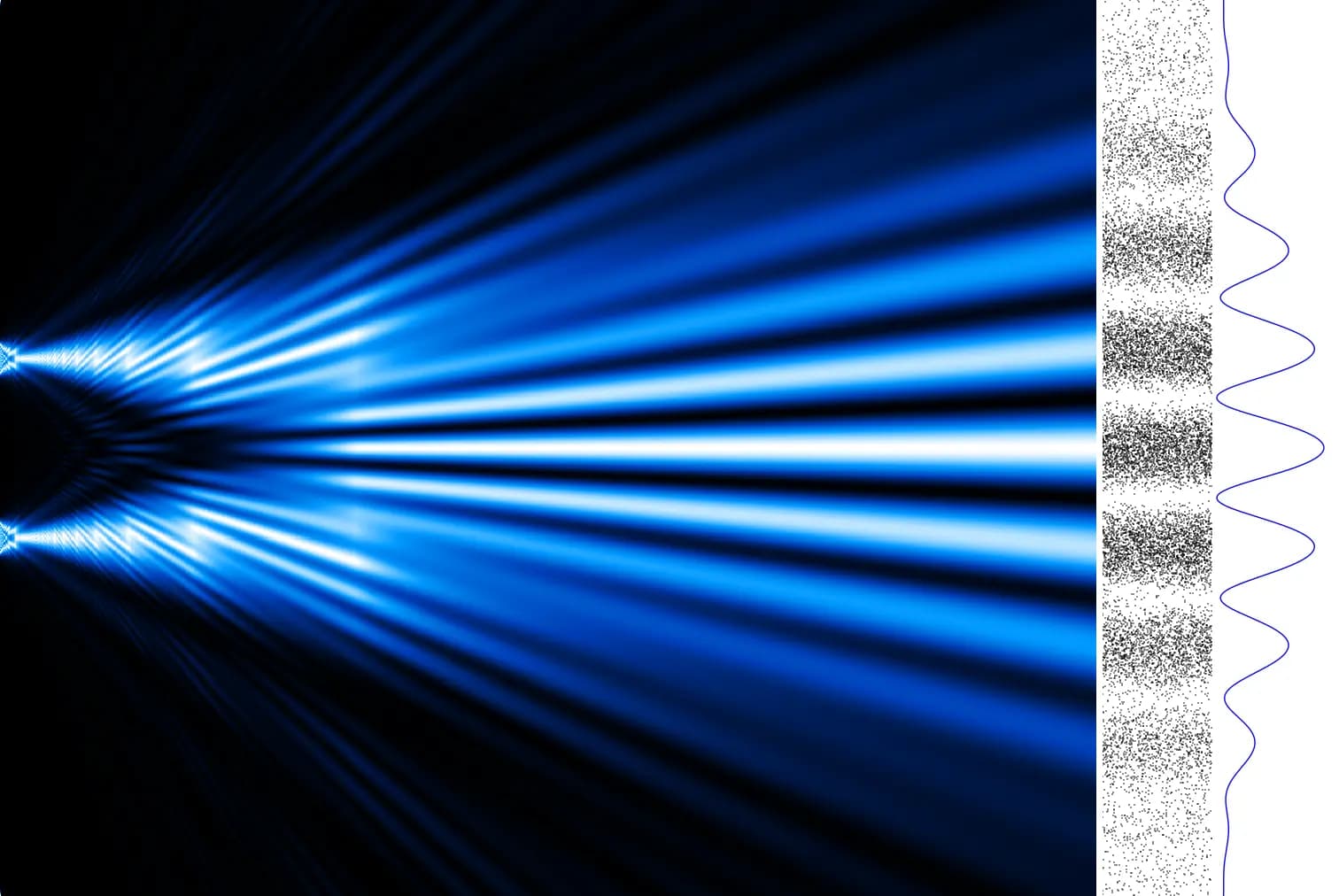
The MIT team aimed to address these limitations by substituting electrical stimulation with ultrasound. Recognizing that most neurons possess ion channels responsive to mechanical stimulation like sound wave vibrations, they saw the potential of ultrasound in eliciting cellular activity. To achieve this, they engineered a hair-thin fiber from a flexible polymer. This fiber features a drum-like ultrasound transducer with a vibrating membrane at its tip. When a small electrical voltage is applied to this membrane, which encapsulates a thin piezoelectric film, it generates ultrasonic waves detectable by nearby cells.
“It’s tissue-safe, there’s no exposed electrode surface, and it’s very low-power, which bodes well for translation to patient use,” says Hou.
The researchers, having demonstrated the ability of this ultrasound device, dubbed ImPULS (Implantable Piezoelectric Ultrasound Stimulator), to activate neurons in the hippocampus of mice, proceeded to implant the fibers into the dopamine-producing substantia nigra. The results were remarkable: they successfully stimulated neurons in the dorsal striatum to produce dopamine.
“Brain stimulation has been one of the most effective, yet least understood, methods used to restore health to the brain. ImPULS gives us the ability to stimulate brain cells with exquisite spatial-temporal resolution and in a manner that doesn’t produce the kind of damage or inflammation as other methods. Seeing its effectiveness in areas like the hippocampus opened an entirely new way for us to deliver precise stimulation to targeted circuits in the brain,” says Steve Ramirez, an assistant professor of psychological and brain sciences at Boston University, a faculty member at B.U.’s Center for Systems Neuroscience, and a study author.
The biocompatible device, including its piezoelectric layer made from a novel ceramic called potassium sodium niobate (KNN), currently relies on an external power source. However, the researchers envision future iterations powered by a small implantable battery and electronics unit.
Furthermore, the team developed a microfabrication process allowing for easy modification of the fiber’s length and thickness, as well as the frequency of the piezoelectric transducer’s sound waves. This customization potential makes the device adaptable for various brain regions.
“We cannot say that the device will give the same effect on every region in the brain, but we can easily and very confidently say that the technology is scalable, and not only for mice. We can also make it bigger for eventual use in humans,” Dagdeviren asserts.
Looking ahead, the researchers plan to investigate the effects of ultrasound stimulation on different brain regions and assess the device’s long-term functionality when implanted for extended periods. They are also exploring the possibility of integrating a microfluidic channel, enabling the device to deliver drugs alongside ultrasound.
Beyond its therapeutic potential for Parkinson’s and other diseases, this ultrasound device holds immense promise as a research tool for unraveling the brain’s mysteries.
“Our goal [is] to provide this as a research tool for the neuroscience community, because we believe that we don’t have enough effective tools to understand the brain,” Dagdeviren concludes. “As device engineers, we are trying to provide new tools so that we can learn more about different regions of the brain.”
The research was supported by the MIT Media Lab Consortium and the Brain and Behavior Foundation Research (BBRF) NARSAD Young Investigator Award.











Responses (0 )