One of the most significant hurdles in developing an effective HIV vaccine has been the virus’s rapid mutation rate, enabling it to evade antibody responses triggered by vaccines. Several years ago, MIT researchers made a breakthrough by showing that administering escalating doses of an HIV vaccine over two weeks could partially overcome this challenge, leading to a greater production of neutralizing antibodies. However, such a multi-dose strategy, delivered within a short timeframe, is impractical for large-scale vaccination campaigns.
Now, in a new study, these researchers have discovered a way to achieve a similar immune response using just two doses, spaced one week apart. The initial, smaller dose primes the immune system, enabling a more potent response to the second, larger dose.
This study, which combined computational modeling with experiments in mice, utilized an HIV envelope protein as the vaccine. A single-dose version of this vaccine is currently undergoing clinical trials. The research team hopes to initiate another study group to evaluate the two-dose schedule.
“By integrating the physical and life sciences, we’ve illuminated fundamental immunological principles that guided the development of this two-dose schedule, mimicking the multi-dose regimen,” explains Arup Chakraborty, the John M. Deutch Institute Professor at MIT and a member of MIT’s Institute for Medical Engineering and Science and the Ragon Institute of MIT, MGH, and Harvard University.
Chakraborty also suggests that this approach could be applicable to vaccines for other diseases. He and Darrell Irvine, a former MIT professor and current professor of immunology and microbiology at the Scripps Research Institute, are the senior authors of the study, published in Science Immunology.
Neutralizing Antibodies
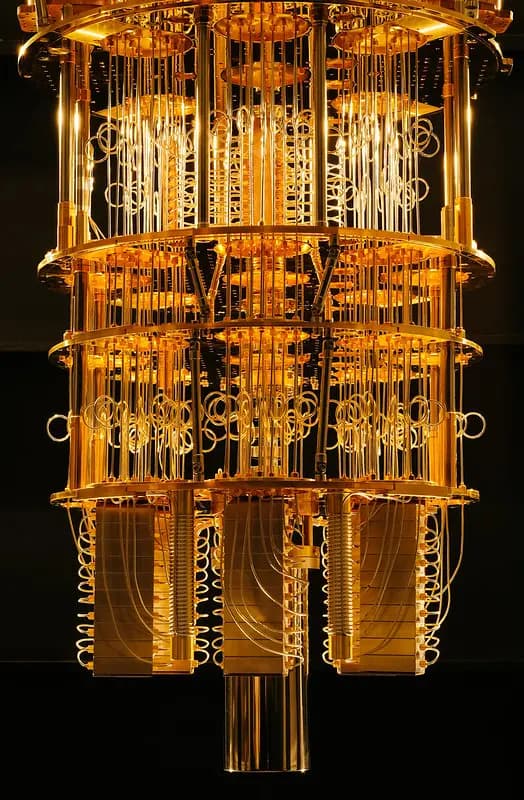
HIV infects over a million people globally each year, with many lacking access to antiviral drugs. An effective vaccine could significantly reduce these infection rates. One promising vaccine candidate, currently in clinical trials, comprises an HIV envelope trimer protein and a nanoparticle adjuvant called SMNP, developed by Irvine’s lab. This nanoparticle enhances the B cell response to the vaccine.
In clinical trials, this and other experimental vaccines have been administered as single doses. However, evidence suggests that a series of doses is more effective in generating broadly neutralizing antibodies. The researchers believe the seven-dose regimen works by mimicking the body’s natural response to viral exposure: a gradual buildup of immune response as viral proteins, or antigens, accumulate.
The MIT team investigated this response dynamic, seeking to replicate the effect with fewer doses. “Administering seven doses is simply not feasible for mass vaccination,” says Sachin Bhagchandani PhD ’23, one of the lead authors. “We aimed to pinpoint the crucial elements behind the escalating dose strategy’s success and determine if that knowledge could help us reduce the number of doses.”
The team compared the effects of one to seven doses, all given within 12 days. Initially, they observed that while three or more doses generated robust antibody responses, two doses did not. However, by adjusting dose intervals and ratios, they found that a first dose of 20% followed by an 80% dose seven days later elicited a response comparable to the seven-dose schedule.
“Understanding the mechanisms driving this phenomenon was clearly critical for future clinical translation,” notes Leerang Yang PhD ’24, another lead author. “Even if the optimal dosing ratio and timing differ in humans, the underlying mechanistic principles are likely to hold true.”
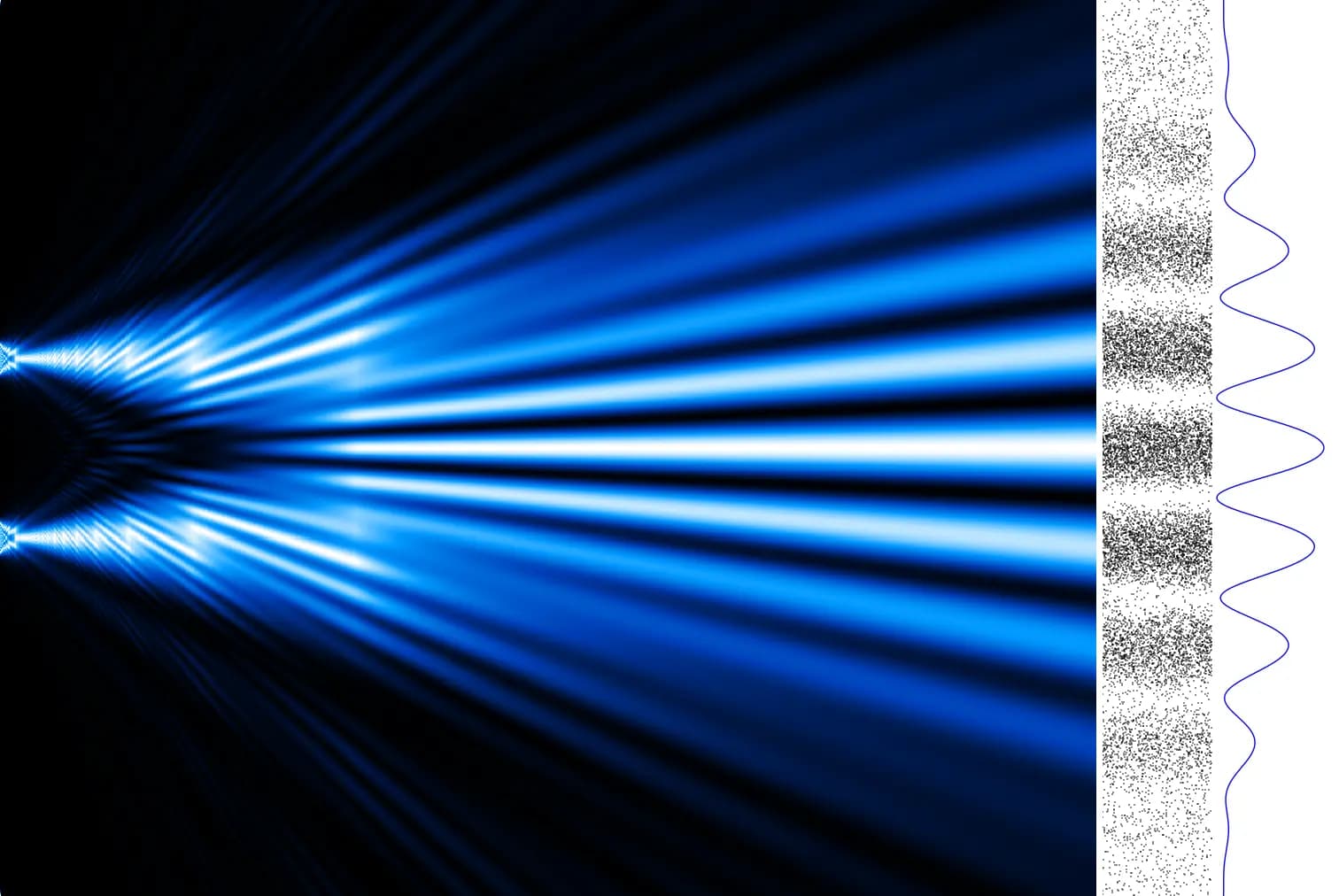
Using a computational model, the researchers analyzed the events unfolding in each dosing scenario. They discovered that a single, full dose resulted in most of the antigen being fragmented before reaching the lymph nodes, where B cells are activated to target specific antigens within germinal centers.
With limited intact antigen reaching the germinal centers, B cells struggle to mount a strong response. However, a small number of B cells do emerge, producing antibodies against the intact antigen. Therefore, a small initial dose primes some B cells and antibody production without “wasting” antigen. When the larger dose follows a week later, these existing antibodies bind to and protect the antigen, escorting it to the lymph node. This increased antigen exposure for B cells ultimately leads to a larger population capable of targeting the virus.
“The early doses generate a small amount of antibody, which is sufficient to bind to and protect the antigen in later doses, guiding it to the lymph node. That’s how we realized that seven doses weren’t necessary,” Bhagchandani explains. “A small initial dose generates this antibody, and when the larger dose is administered, it’s protected by the antibody, which binds to it and transports it to the lymph node.”
T-Cell Boost
These antigens can persist within germinal centers for weeks or longer, providing sustained exposure for B cells and promoting the development of diverse antibody types.
The two-dose schedule also demonstrated a stronger T-cell response. The first dose activates dendritic cells, which stimulate inflammation and T-cell activation. The second dose further amplifies this effect, boosting the T-cell response.
Overall, compared to a single dose, the two-dose regimen resulted in a fivefold increase in T-cell response and a 60-fold improvement in antibody response.
“Reducing the ‘escalating dose’ strategy to just two shots makes it far more practical for clinical implementation. Moreover, several technologies under development could potentially replicate the two-dose exposure in a single shot, which would be ideal for mass vaccination campaigns,” says Irvine.
The researchers are currently evaluating this vaccine strategy in a nonhuman primate model. They are also developing specialized materials for extended release of the second dose, potentially further enhancing the immune response.
This research was supported by the Koch Institute Support (core) Grant from the National Cancer Institute, the National Institutes of Health, and the Ragon Institute of MIT, MGH, and Harvard.











Responses (0 )