Anesthesiologists have a range of drugs at their disposal to render patients unconscious, but the precise mechanisms by which these drugs affect the brain have remained a mystery. Now, MIT neuroscientists have shed light on this process for the widely used anesthetic drug, propofol. Their groundbreaking research reveals that propofol tips the delicate balance of the brain’s activity, pushing it towards instability until consciousness fades.
The brain has to operate on this knife’s edge between excitability and chaos. It’s got to be excitable enough for its neurons to influence one another, but if it gets too excitable, it spins off into chaos. Propofol seems to disrupt the mechanisms that keep the brain in that narrow operating range,
explains Earl K. Miller, the Picower Professor of Neuroscience and a member of MIT’s Picower Institute for Learning and Memory. Published in Neuron, the study holds promising implications for developing advanced monitoring tools for patients undergoing general anesthesia. The research was led by Miller and Ila Fiete, a professor of brain and cognitive sciences, the director of the K. Lisa Yang Integrative Computational Neuroscience Center (ICoN), and a member of MIT’s McGovern Institute for Brain Research. MIT graduate student Adam Eisen and MIT postdoc Leo Kozachkov were the lead authors of the paper.
Propofol works by binding to GABA receptors in the brain, effectively inhibiting the neurons equipped with these receptors. While other anesthetic drugs target different receptor types, the universal mechanism behind their ability to induce unconsciousness has been elusive.
The research team, headed by Miller and Fiete, proposed that propofol, and potentially other anesthetic agents, disrupt a critical brain state known as “dynamic stability.” This state allows neurons to remain receptive to new information while ensuring the brain can swiftly regain control and prevent excessive excitation.
Previous attempts to unravel the effects of anesthesia on this delicate balance have yielded conflicting results. Some studies suggest that anesthesia pushes the brain towards excessive stability and unresponsiveness, ultimately leading to unconsciousness. Conversely, others pointed to heightened excitability and a chaotic brain state as the culprit behind the loss of consciousness.
These inconsistencies stemmed partly from the difficulty in accurately measuring dynamic stability within the brain. The ability to track dynamic stability as consciousness fades would provide crucial insights into whether unconsciousness arises from too much or too little stability.
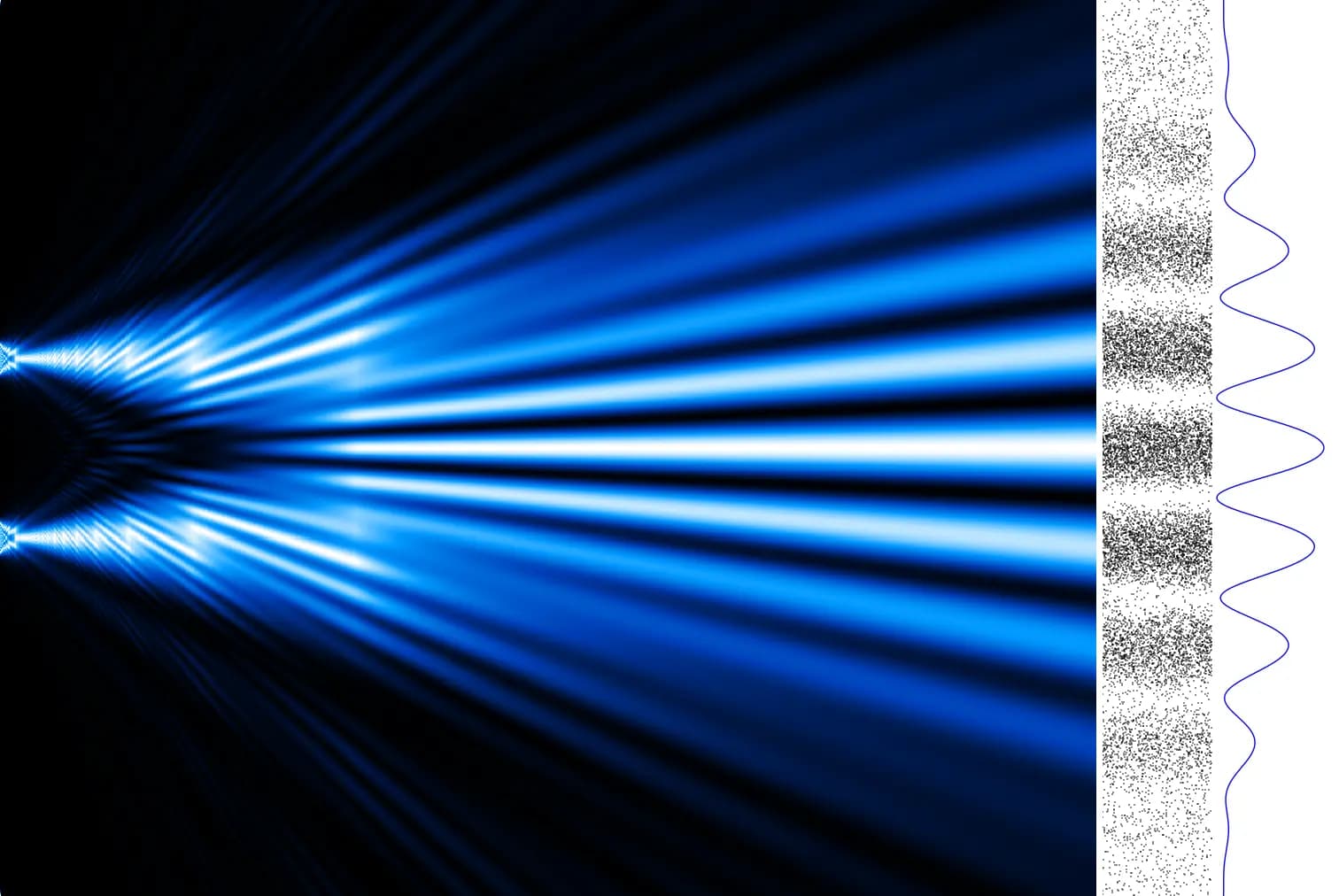
To address this challenge, the researchers analyzed electrical recordings from the brains of animals receiving propofol over an hour. During this period, the animals gradually slipped into unconsciousness. The recordings targeted four brain regions associated with vision, sound processing, spatial awareness, and executive function.
Recognizing that these recordings represented a minuscule fraction of the brain’s overall activity, the researchers employed a technique called delay embedding. This method enabled them to characterize dynamical systems from limited measurements by supplementing each measurement with previously recorded data.
Armed with this approach, the researchers quantified the brain’s response to sensory inputs, such as sounds, and spontaneous fluctuations in neural activity.
In the awake state, neural activity typically spikes after an input and then gracefully returns to its baseline. However, as propofol administration began, the brain exhibited a delayed return to baseline following these inputs, indicating a lingering state of heightened excitation. This effect intensified progressively until the animals succumbed to unconsciousness.
These findings strongly suggest that propofol’s inhibition of neuronal activity triggers escalating instability, ultimately culminating in the loss of consciousness.
To validate their observations, the researchers constructed a simplified neural network model. By increasing the inhibition of specific nodes within the network, mimicking propofol’s action in the brain, they observed a destabilization of network activity, mirroring the unstable patterns observed in the brains of animals under propofol.
We looked at a simple circuit model of interconnected neurons, and when we turned up inhibition in that, we saw a destabilization. So, one of the things we’re suggesting is that an increase in inhibition can generate instability, and that is subsequently tied to loss of consciousness,
states Eisen.
Fiete elaborates, “This paradoxical effect, in which boosting inhibition destabilizes the network rather than silencing or stabilizing it, occurs because of disinhibition. When propofol boosts the inhibitory drive, this drive inhibits other inhibitory neurons, and the result is an overall increase in brain activity.”
The researchers hypothesize that other anesthetic drugs, despite targeting different neuron and receptor types, might converge on this same effect through distinct mechanisms. This intriguing possibility is currently under investigation.
Should this hypothesis prove true, it could significantly advance ongoing efforts to develop more precise control over anesthesia levels during patient care. Miller, in collaboration with Emery Brown, the Edward Hood Taplin Professor of Medical Engineering at MIT, is actively working on systems that monitor brain dynamics and adjust drug dosages in real time.
“If you find common mechanisms at work across different anesthetics, you can make them all safer by tweaking a few knobs, instead of having to develop safety protocols for all the different anesthetics one at a time,” Miller points out. “You don’t want a different system for every anesthetic they’re going to use in the operating room. You want one that’ll do it all.”
Beyond anesthesia, the researchers envision applying their dynamic stability measurement technique to other brain states, including neuropsychiatric disorders.
“This method is pretty powerful, and I think it’s going to be very exciting to apply it to different brain states, different types of anesthetics, and also other neuropsychiatric conditions like depression and schizophrenia,” Fiete concludes.
The research was made possible by funding from the Office of Naval Research, the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, the National Science Foundation Directorate for Computer and Information Science and Engineering, the Simons Center for the Social Brain, the Simons Collaboration on the Global Brain, the JPB Foundation, the McGovern Institute, and the Picower Institute.











Responses (0 )