Many vaccines, including vaccines for hepatitis B and whooping cough, consist of fragments of viral or bacterial proteins. These vaccines often include other molecules called adjuvants, which help to boost the immune system’s response to the protein.
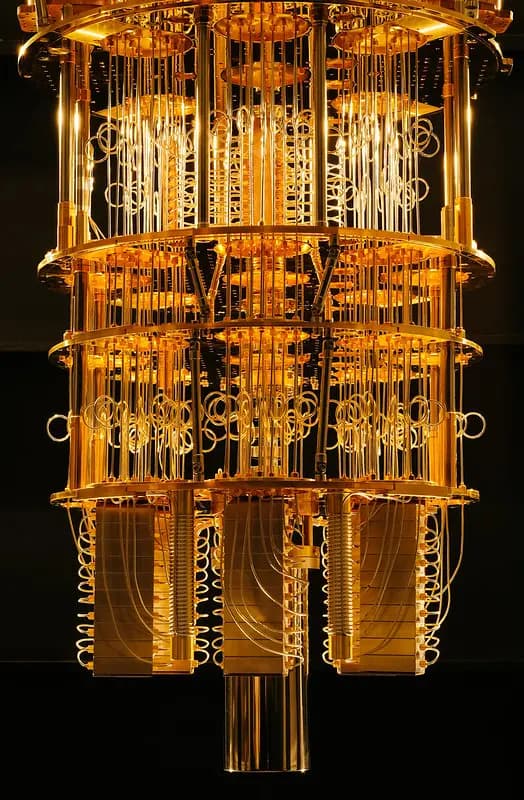
Most of these adjuvants consist of aluminum salts or other molecules that provoke a nonspecific immune response. A team of MIT researchers has now shown that a type of nanoparticle called a metal-organic framework (MOF) can also provoke a strong immune response, by activating the innate immune system — the body’s first line of defense against any pathogen — through cell proteins called toll-like receptors.
In a study of mice, the researchers showed that this MOF could successfully encapsulate and deliver part of the SARS-CoV-2 spike protein, while also acting as an adjuvant once the MOF is broken down inside cells.
While more work would be needed to adapt these particles for use as vaccines, the study demonstrates that this type of structure can be useful for generating a strong immune response, the researchers say.
Understanding how the drug delivery vehicle can enhance an adjuvant immune response is something that could be very helpful in designing new vaccines,
says Ana Jaklenec, a principal investigator at MIT’s Koch Institute for Integrative Cancer Research and one of the senior authors of the new study.
Robert Langer, an MIT Institute Professor and member of the Koch Institute, and Dan Barouch, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center and a professor at Harvard Medical School, are also senior authors of the paper, which appears today in Science Advances. The paper’s lead author is former MIT postdoc and Ibn Khaldun Fellow Shahad Alsaiari.
Immune activation
In this study, the researchers focused on an MOF called ZIF-8, which consists of a lattice of tetrahedral units made up of a zinc ion attached to four molecules of imidazole, an organic compound. Previous work has shown that ZIF-8 can significantly boost immune responses, but it wasn’t known exactly how this particle activates the immune system.
To try to figure that out, the MIT team created an experimental vaccine consisting of the SARS-CoV-2 receptor-binding protein (RBD) embedded within ZIF-8 particles. These particles are between 100 and 200 nanometers in diameter, a size that allows them to get into the body’s lymph nodes directly or through immune cells such as macrophages.
Once the particles enter the cells, the MOFs are broken down, releasing the viral proteins. The researchers found that the imidazole components then activate toll-like receptors (TLRs), which help to stimulate the innate immune response.
“This process is analogous to establishing a covert operative team at the molecular level to transport essential elements of the COVID-19 virus to the body’s immune system, where they can activate specific immune responses to boost vaccine efficacy,” Alsaiari says.
RNA sequencing of cells from the lymph nodes showed that mice vaccinated with ZIF-8 particles carrying the viral protein strongly activated a TLR pathway known as TLR-7, which led to greater production of cytokines and other molecules involved in inflammation.
Mice vaccinated with these particles generated a much stronger response to the viral protein than mice that received the protein on its own.
“Not only are we delivering the protein in a more controlled way through a nanoparticle, but the compositional structure of this particle is also acting as an adjuvant,” Jaklenec says. “We were able to achieve very specific responses to the Covid protein, and with a dose-sparing effect compared to using the protein by itself to vaccinate.”
Vaccine access
While this study and others have demonstrated ZIF-8’s immunogenic ability, more work needs to be done to evaluate the particles’ safety and potential to be scaled up for large-scale manufacturing. If ZIF-8 is not developed as a vaccine carrier, the findings from the study should help to guide researchers in developing similar nanoparticles that could be used to deliver subunit vaccines, Jaklenec says.
“Most subunit vaccines usually have two separate components: an antigen and an adjuvant,” Jaklenec says. “Designing new vaccines that utilize nanoparticles with specific chemical moieties which not only aid in antigen delivery but can also activate particular immune pathways have the potential to enhance vaccine potency.”
One advantage to developing a subunit vaccine for COVID-19 is that such vaccines are usually easier and cheaper to manufacture than mRNA vaccines, which could make it easier to distribute them around the world, the researchers say.
“Subunit vaccines have been around for a long time, and they tend to be cheaper to produce, so that opens up more access to vaccines, especially in times of pandemic,” Jaklenec says.
The research was funded by Ibn Khaldun Fellowships for Saudi Arabian Women and in part by the Koch Institute Support (core) Grant from the U.S. National Cancer Institute.
The link to the original article can be found here.











Responses (0 )